Cardiac Rehabilitation At A Glance

What are the benefits of cardiac rehabilitation?
- Individuals who attend 36 sessions have a 47% lower risk of death and a 31% lower risk of heart attack than those who attend only 1 session.
- Health systems save $4,950 to $9,200 per person per year of life saved.
- Cardiac rehab participation also reduces hospital readmissions.

Who can benefit but is not being referred?
- Minority status predicts lower referral and participation rates.
- Women, minorities, older people, and those with other medical conditions are under-referred to cardiac rehab.
- One of the best predictors of cardiac rehab referral is whether the eligible person speaks English. Asian Americans are 18 times more likely than white people to speak limited English.
- Black women are 60% less likely than white women to be referred and enroll in cardiac rehab programs.

What improves cardiac rehab referral rates?
- Automatic, systematic referral to cardiac rehab at discharge can help connect eligible people with these programs.
- Strong coordination among inpatient, home health, and outpatient cardiac rehab programs boosts referral rates as well as participation rates and outcomes.
- Patients’ medical teams and families can support and encourage participation in cardiac rehab programs.
- Awareness campaigns should be aimed at people and caregivers.

What are the barriers to cardiac rehabilitation participation and completion?
- Longer wait times following discharge reduce cardiac rehab enrollment.
- For every day a person waits to start cardiac rehab, that person is 1% less likely to enroll.
- People who live outside of metropolitan areas are 30% less likely to participate in cardiac rehab programs.
- People who make more than $75,000 per year are twice as likely to participate as individuals with annual incomes below $15,000.
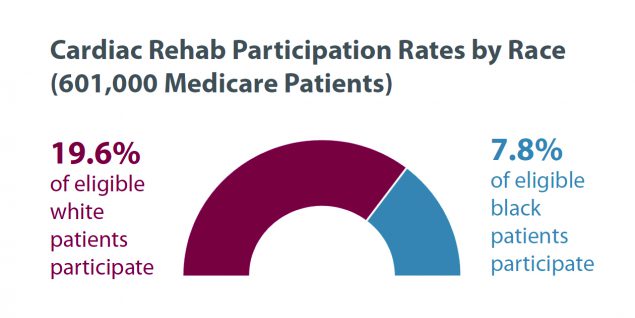
- Race matters:

How do health systems eliminate barriers to cardiac rehabilitation participation and completion?
- The greatest predictor of participation is the strength of the physician’s recommendation.
- Reduce the interval between hospital discharge and cardiac rehab program orientation by formalizing enrollment practices.
- Support participation in cardiac rehab through community health workers, home health aides, and visiting nurses.
- Design culturally and linguistically appropriate programs.
- Increase use of translation services by physicians and participants.
- Ensure access to services through transportation options and extended hours.
- Where possible, reduce or eliminate financial burden on cardiac rehab participants.
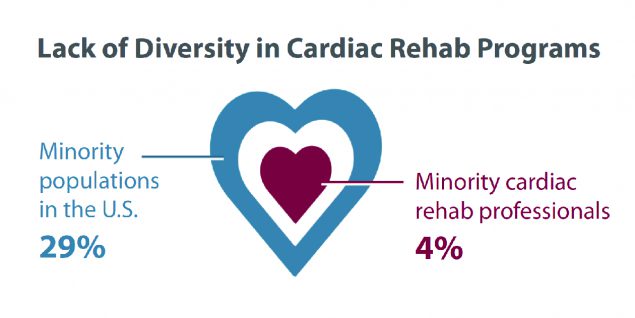
- Diversify cardiac rehab teams.
- Research shows that minority physicians are more likely than white physicians to care for minority, low-income, uninsured, and underserved people.

What other strategies and delivery models could help cardiac rehabilitation uptake?
- Create web-based or home-based programs in rural areas.
- Develop telemedicine-monitored cardiac rehab programs for people unable to access traditional programs.
- For people unable to attend all 36 sessions in a cardiac rehab facility, conduct baseline assessment in a cardiac rehab clinic followed by a nurse-monitored home exercise program.
- Reward eligible people for completing cardiac rehab programs.
- Reward programs with high completion rates.
- Share best practices and lessons learned, including innovations.

A Limited Capacity Limits the Number of Eligible People Served
Complicating the story of program capacity are the geographic variations in the number of
- Cardiac rehab programs
- Eligible people
- Referred and participating people
Although cardiac rehab programs are underutilized, some fear that the existing number of programs would be insufficient to serve all eligible people.

Download and share an infographic on this content with your audiences.
Additional Resources
- Cardiac Rehabilitation
Learn about what cardiac rehabilitation involves and why patients who have had a cardiac event should incorporate cardiac rehabilitation into their lives. This page also has a list of tools for clinicians, cardiac rehabilitation teams, and patients, including key publications and guidelines on the subject. - Cardiac Rehabilitation: Change Package
This change package is a quality improvement tool to help teams from hospitals and cardiac rehabilitation programs put systems and strategies in place that target improved care for more eligible patients. It presents a listing of process improvements that cardiac rehabilitation champions can implement and includes change concepts, change ideas, and tools and resources. - Cardiac Rehabilitation Communications Kit
This communications kit will equip your organization with resources and messages to spread awareness about the value of cardiac rehabilitation and solutions for increasing participation. - Million Hearts® #CardiacRehabChat Twitter Moments
Explore resources for improving enrollment, engagement, and adherence shared during our #CardiacRehabChat series.
